Prednisone, a corticosteroid, treats inflammation and suppresses the immune system. Doctors prescribe it for various conditions requiring rapid symptom relief. Think autoimmune diseases like rheumatoid arthritis, lupus, or inflammatory bowel disease where it powerfully reduces swelling and pain.
Beyond autoimmune conditions, prednisone effectively manages allergic reactions, asthma exacerbations, and certain cancers. For example, in severe allergic reactions, it quickly counteracts inflammation, preventing life-threatening complications. Similarly, during severe asthma attacks, it opens airways and eases breathing.
Furthermore, it’s often a part of treatment plans for conditions like multiple sclerosis and certain types of eye inflammation, significantly improving patients’ quality of life. However, it’s crucial to remember that prednisone has potential side effects, so close monitoring by a physician is necessary. Always discuss the risks and benefits with your doctor before starting this medication.
Remember: Prednisone is a powerful medication. Never self-medicate or alter prescribed dosage. Consult your healthcare provider for appropriate use and management of potential side effects.
- Why Would Prednisone Be Prescribed?
- Autoimmune Diseases: Managing Inflammation
- Conditions Responsive to Prednisone
- Understanding the Treatment
- Lifestyle Adjustments
- Allergic Reactions: Suppressing Immune Response
- Targeting Inflammatory Pathways
- Dosage and Duration
- Asthma: Reducing Airway Inflammation
- Chronic Obstructive Pulmonary Disease (COPD): Managing Exacerbations
- Short-Term Prednisone Use
- Beyond Prednisone: A Multifaceted Approach
- Long-Term COPD Management
- When to Seek Immediate Medical Attention
- Lupus: Controlling Symptoms and Flare-ups
- Rheumatoid Arthritis: Reducing Joint Pain and Swelling
- Managing RA Symptoms with Prednisone
- Understanding Prednisone’s Role in a Treatment Plan
- Lifestyle Modifications for RA
- Inflammatory Bowel Disease (IBD): Managing Symptoms
- Dietary Adjustments for IBD
- Lifestyle Modifications and Stress Management
- Medication Beyond Prednisone
- Cancer Treatment: Reducing Swelling and Side Effects
Why Would Prednisone Be Prescribed?
Prednisone, a corticosteroid, powerfully reduces inflammation and suppresses the immune system. Doctors prescribe it for a variety of conditions requiring these actions.
- Autoimmune diseases: Prednisone helps manage conditions like lupus, rheumatoid arthritis, and inflammatory bowel disease by dampening the immune response attacking the body’s own tissues.
- Allergic reactions: Severe allergic reactions, such as anaphylaxis, often necessitate prednisone to rapidly reduce inflammation and prevent life-threatening complications.
- Asthma and COPD: It reduces airway inflammation, improving breathing in these conditions. This can be especially helpful during exacerbations.
- Skin conditions: Severe eczema, psoriasis, and other inflammatory skin diseases benefit from prednisone’s anti-inflammatory properties.
- Certain cancers: In some cases, prednisone is used in conjunction with chemotherapy or radiation therapy to manage symptoms and reduce tumor size.
- Organ transplantation: Prednisone is often a part of the immunosuppressive regimen following organ transplantation to prevent rejection.
- Inflammatory eye conditions: Conditions like uveitis often require prednisone to reduce inflammation and protect vision.
- Other inflammatory conditions: Prednisone finds use in treating various other inflammatory diseases, including multiple sclerosis and temporal arteritis.
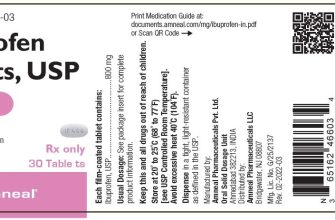
Remember: Prednisone has significant side effects, and long-term use requires careful monitoring by a physician. Always discuss potential risks and benefits with your doctor before taking this medication.
- Discuss your medical history completely with your doctor.
- Follow your doctor’s prescribed dosage precisely.
- Report any side effects immediately.
- Never stop taking prednisone abruptly without consulting your physician.
Autoimmune Diseases: Managing Inflammation
Prednisone, a corticosteroid, powerfully reduces inflammation in autoimmune diseases. It works by suppressing the immune system’s overactive response, lessening the damage to your body’s tissues.
Conditions Responsive to Prednisone
Many autoimmune conditions benefit from prednisone. Rheumatoid arthritis, lupus, and inflammatory bowel disease often see significant symptom improvement with prednisone treatment. The medication also aids in managing conditions like multiple sclerosis and dermatomyositis by tackling inflammation.
Understanding the Treatment
Your doctor carefully determines the correct prednisone dosage based on your specific condition and its severity. They will monitor you closely for side effects, which can include weight gain, increased blood sugar, and mood changes. Tapering off prednisone gradually is essential to minimize withdrawal symptoms.
Remember, prednisone isn’t a cure; it manages symptoms. Long-term use comes with risks, so your doctor might prescribe it for flare-ups or as part of a combination therapy alongside disease-modifying antirheumatic drugs (DMARDs) or biologics for better long-term disease management.
Lifestyle Adjustments
Alongside medication, lifestyle changes support autoimmune disease management. Regular exercise helps manage inflammation and weight, while a balanced diet low in processed foods and rich in fruits, vegetables, and whole grains provides your body with the support it needs to heal.
Allergic Reactions: Suppressing Immune Response
Prednisone effectively combats severe allergic reactions by dampening the immune system’s overreaction. This powerful corticosteroid reduces inflammation and suppresses the release of histamine and other inflammatory chemicals responsible for symptoms like swelling, itching, and difficulty breathing.
Targeting Inflammatory Pathways
Prednisone works by binding to specific receptors within immune cells, hindering the production of inflammatory molecules like cytokines. This action directly interferes with the signaling pathways that trigger and amplify the allergic response. The reduction in inflammation provides significant relief from allergy symptoms.
Dosage and Duration
Doctors carefully determine the appropriate prednisone dosage and treatment duration based on the severity of the allergic reaction and the patient’s overall health. Short-term use is generally preferred to minimize potential side effects. Always follow your doctor’s instructions precisely.
Asthma: Reducing Airway Inflammation
Prednisone helps control asthma by powerfully reducing airway inflammation. This corticosteroid significantly decreases the swelling and irritation in your bronchial tubes, allowing you to breathe easier. It acts quickly, offering relief from symptoms like wheezing and coughing.
The medication works by suppressing the body’s inflammatory response. This means it reduces the production of inflammatory chemicals, such as leukotrienes and prostaglandins, that contribute to asthma attacks. A course of prednisone, therefore, provides rapid symptom control during an exacerbation.
Important Note: Prednisone is typically used for short-term treatment of asthma flares. Long-term use carries risks, so always follow your doctor’s instructions carefully. Your physician may recommend a combination of inhaled corticosteroids for daily maintenance alongside prednisone during flare-ups to manage asthma effectively and minimize side effects.
Remember: This information does not replace advice from your doctor. Discuss your asthma management plan with your healthcare provider to determine the best course of action for you.
Chronic Obstructive Pulmonary Disease (COPD): Managing Exacerbations
Prednisone, a corticosteroid, frequently treats COPD exacerbations. It reduces airway inflammation, easing breathing difficulties. However, long-term use carries risks, so it’s typically used for short bursts.
Short-Term Prednisone Use
Doctors usually prescribe a course of prednisone lasting 5-10 days. Higher doses might be needed initially, followed by a gradual tapering. This helps minimize side effects while still providing effective relief. Close monitoring by your physician is crucial.
- Typical Dosage: The precise dosage depends on the severity of your exacerbation. Your doctor will determine the appropriate amount.
- Side Effects: Common side effects include increased appetite, weight gain, mood changes, and insomnia. Rare, but serious, side effects include increased blood sugar and increased risk of infection. Report any concerning symptoms to your doctor immediately.
- Tapering: Stopping prednisone abruptly can cause symptoms to return or worsen. Your doctor will create a tapering schedule to gradually reduce the dosage.
Beyond Prednisone: A Multifaceted Approach
Prednisone is often part of a broader treatment plan for COPD exacerbations. Additional therapies may include:
- Bronchodilators: These medications relax the airway muscles, making it easier to breathe. They can be inhaled or taken orally.
- Antibiotics: If an infection is causing the exacerbation, antibiotics will be prescribed. The choice of antibiotic will depend on the suspected bacteria.
- Oxygen Therapy: Supplemental oxygen may be necessary to improve blood oxygen levels, particularly during severe exacerbations.
Long-Term COPD Management
Managing COPD successfully involves more than just treating exacerbations. Regular use of maintenance medications, pulmonary rehabilitation, and lifestyle changes like smoking cessation are equally important. Discuss a long-term management plan with your physician to minimize future exacerbations and improve your quality of life.
When to Seek Immediate Medical Attention
During a COPD exacerbation, promptly seek medical attention if you experience: increased shortness of breath, worsening cough, increased sputum production (especially if it changes color), or fever.
Lupus: Controlling Symptoms and Flare-ups
Prednisone often helps manage lupus symptoms. It reduces inflammation, easing pain and swelling in joints and other affected areas. However, long-term use has drawbacks, so doctors often combine it with other medications.
Hydroxychloroquine is a common addition to a prednisone regimen. It helps prevent flare-ups and slows disease progression. Regular blood tests monitor for side effects.
Lifestyle adjustments play a vital role. Protecting your skin from sun exposure is crucial – UV radiation can trigger flares. A balanced diet, regular exercise, and stress management techniques significantly improve overall well-being.
Biologics, such as belimumab or rituximab, are powerful medications reserved for more severe cases. They target specific parts of the immune system contributing to lupus. Careful monitoring is necessary, as these drugs can cause side effects.
Regular checkups with your rheumatologist are non-negotiable. They allow for close monitoring of your condition, timely adjustments to your medication, and prompt management of any new symptoms.
Managing lupus requires a team approach. Open communication with your doctor and other healthcare professionals ensures the most effective treatment plan tailored to your specific needs and situation.
Rheumatoid Arthritis: Reducing Joint Pain and Swelling
Prednisone, a corticosteroid, effectively reduces inflammation in rheumatoid arthritis (RA). It’s often prescribed to quickly alleviate severe symptoms like pain and swelling.
Managing RA Symptoms with Prednisone
Prednisone works by suppressing the immune system’s response that causes joint inflammation. This leads to noticeable improvements in joint pain, stiffness, and swelling within days of starting treatment. However, it’s crucial to remember that prednisone is usually a short-term solution, and long-term use carries potential side effects.
Alongside prednisone, your doctor will likely recommend other therapies. These might include disease-modifying antirheumatic drugs (DMARDs) to slow disease progression, or biologic medications targeting specific immune system components. Physical therapy also plays a significant role in maintaining joint mobility and strengthening muscles.
Understanding Prednisone’s Role in a Treatment Plan
Your doctor will create a personalized treatment plan that balances the benefits of prednisone with its potential risks. They will carefully monitor your response to the medication and adjust the dosage as needed. Regular blood tests are often part of this monitoring process.
| Treatment Aspect | Action |
|---|---|
| Pain Management | Prednisone reduces inflammation, leading to pain relief. Additional pain relievers may be prescribed. |
| Swelling Reduction | Prednisone directly targets the inflammation causing swelling in joints. |
| Long-Term Management | DMARDs and biologics slow disease progression, while physical therapy helps maintain function. |
| Medication Monitoring | Regular blood tests track your response to prednisone and ensure safe use. |
Lifestyle Modifications for RA
Maintaining a healthy lifestyle complements your medical treatment. A balanced diet, regular low-impact exercise, and stress management techniques can all positively impact RA symptoms. Consistent adherence to your prescribed treatment plan is key to long-term success.
Inflammatory Bowel Disease (IBD): Managing Symptoms
Prednisone, a corticosteroid, significantly reduces inflammation, offering quick relief from IBD symptoms like abdominal pain, diarrhea, and urgency. However, it’s usually a short-term solution due to potential side effects.
Dietary Adjustments for IBD
Specific dietary changes can greatly impact symptom management. Eliminating trigger foods, such as dairy, gluten, or high-fiber items, may be necessary for some individuals. Working with a registered dietitian helps create a personalized, nutritionally balanced plan. Small, frequent meals often improve tolerance.
Lifestyle Modifications and Stress Management
Stress exacerbates IBD. Incorporating stress-reduction techniques, such as yoga, meditation, or deep breathing exercises, may prove beneficial. Regular, moderate exercise supports overall health and well-being, but should be adjusted to accommodate current symptom levels. Adequate sleep is also critical for symptom control.
Medication Beyond Prednisone
Beyond prednisone, other medications like aminosalicylates (mesalamine) and immunomodulators (azathioprine, 6-mercaptopurine) help control inflammation long-term. Biologic therapies (infliximab, adalimumab) are potent agents targeting specific immune pathways, offering substantial relief for those with moderate-to-severe IBD. Your gastroenterologist will determine the most suitable treatment strategy.
Cancer Treatment: Reducing Swelling and Side Effects
Prednisone helps manage swelling (edema) caused by cancer or its treatment. This reduction in swelling improves patient comfort.
Chemotherapy and radiation often cause inflammation. Prednisone’s anti-inflammatory properties alleviate these side effects, leading to better quality of life for patients undergoing treatment.
Certain cancers, like leukemia, cause significant swelling and organ enlargement. Prednisone shrinks these areas, relieving pressure and improving organ function.
Beyond swelling, prednisone mitigates nausea and vomiting, common side effects of cancer therapies. This helps patients maintain adequate nutrition and hydration.
Note: Prednisone has potential side effects. Discuss these with your oncologist to weigh benefits against risks specific to your situation. They will adjust dosage and monitor for potential complications.